Minimally Invasive Total Knee Arthroplasty (MIS TKA) is a technique aimed at reducing the size of the incision and minimizing trauma to the surrounding tissues during knee replacement surgery. This procedure involves replacing a damaged or arthritic knee joint with a prosthetic implant using smaller incisions and refined techniques. Here’s a detailed explanation of the procedure:
Preoperative Preparation
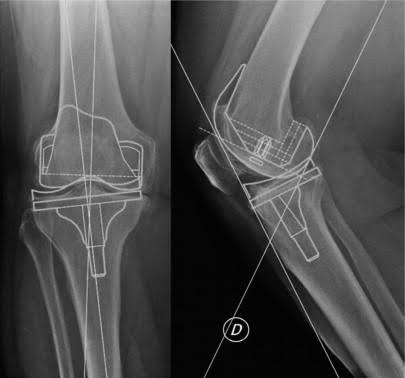
Imaging & Planning: In some cases, advanced imaging techniques like X-rays or CT scans are used to plan the surgery with precision. Some surgeons may use robotic-assisted systems to guide the procedure and ensure accurate placement of the prosthesis.
Anesthesia: The patient is usually given regional anesthesia (spinal or epidural block) to numb the lower half of the body.
Positioning: The patient is positioned on the operating table, with the knee exposed for the procedure. The leg is prepped and draped in a sterile manner.
Incision
- Minimal Incision: The key difference in MIS TKA is the smaller incision. Typically, an incision of around 3 to 4 inches (as opposed to the traditional 6 to 8-inch incision) is made on the front of the knee. This is done using specialized instruments and careful technique.
- Skin and Soft Tissue Dissection: The incision is carefully made, and the surgeon moves the skin, fat, and other soft tissues to expose the knee joint. The quadriceps muscle and tendon are either gently displaced or partially incised, depending on the surgeon’s approach.
Exposure of the Knee Joint
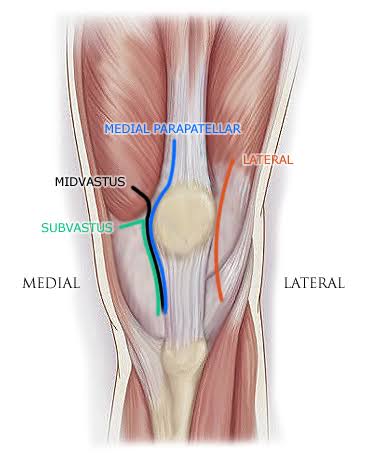
- Accessing the Joint: The surgeon uses specialized retractors to gently move the surrounding soft tissues, including muscles, tendons, and ligaments, without causing significant damage. In MIS TKA, there is minimal disruption of the quadriceps muscle and tendon, which are the primary structures at the front of the knee.
- Preserving the Ligaments: The anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL) may be preserved depending on the type of prosthesis being used and the surgeon’s approach. In some cases, the PCL is removed if necessary for the type of implant chosen.
Bone Preparation
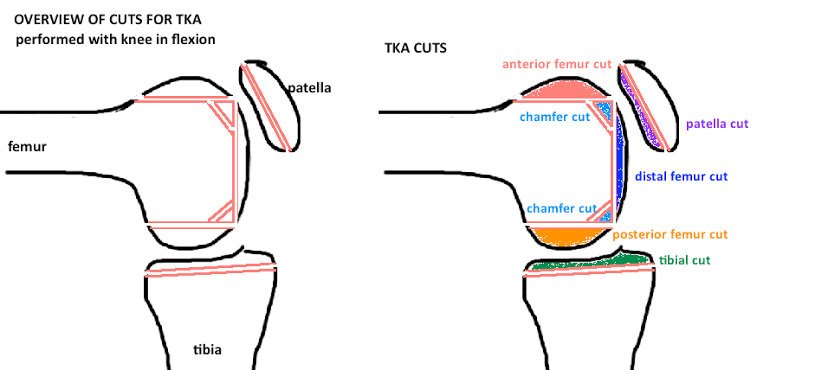
- Resection of Damaged Bone: The surgeon removes the damaged surfaces of the femur (thigh bone), tibia (shin bone), and sometimes the patella (kneecap). Precision instruments are used to cut the bones to accommodate the prosthetic components, ensuring that the alignment and angles of the joint are optimized for proper function.
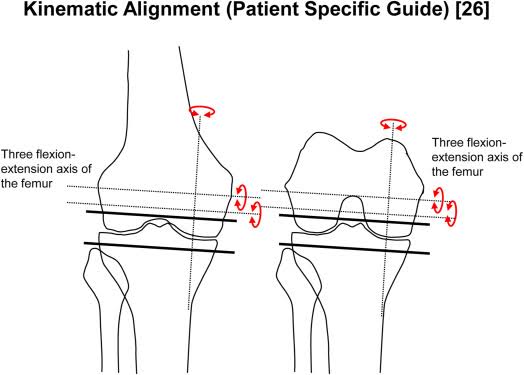
- Alignment Guides: Surgeons may use alignment guides to ensure that the bone cuts are precise. This step is crucial for achieving proper knee function post-surgery and for the longevity of the implant.
Implantation of the Prosthesis
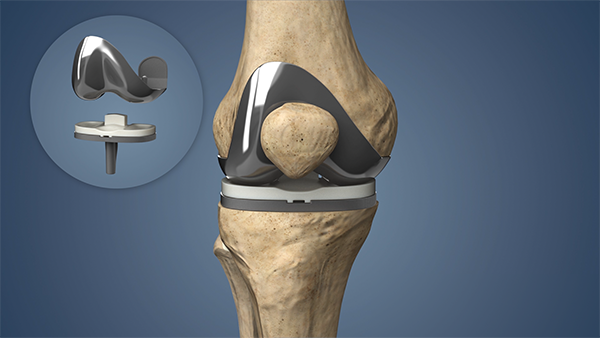
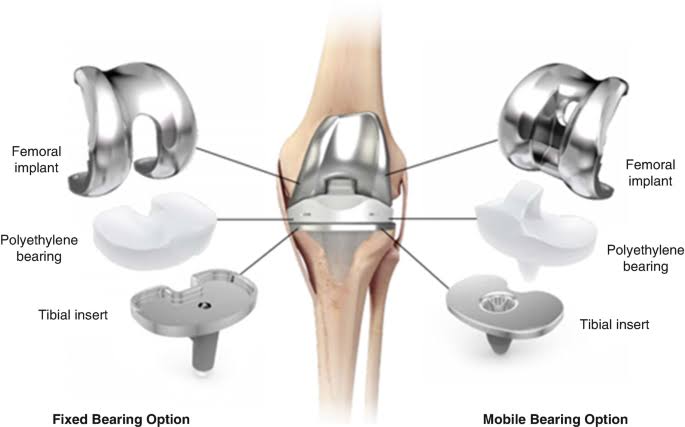
- Prosthetic Components: Once the bone is prepared, the surgeon inserts the prosthetic components:
- The femoral component is placed on the end of the femur.
- The tibial component is placed on the tibia.
- A polyethylene insert (the bearing surface) is placed between the femoral and tibial components to allow smooth movement.
Final Adjustments and Securing the Implant
- Securing the Implant: Once the trial components are deemed to be in proper alignment, the surgeon removes the trial components and permanently secures the prosthetic components using bone cement or press-fit technology (depending on the type of prosthesis).
- Testing Range of Motion: After securing the components, the knee is tested to ensure that the joint moves smoothly, has proper stability, and achieves the desired range of motion.
Closing the Incision
- Wound Closure: The incision is closed using sutures or staples. In some cases, absorbable sutures are used for internal closure, while the skin may be closed with either sutures or a special adhesive.
- Dressing and Bandage: A sterile dressing is applied to the incision site to protect it from infection and absorb any drainage.
Postoperative Care
- Recovery Room: After the surgery, the patient is moved to the recovery room where they are monitored as they wake up from anesthesia.
- Pain Management: Pain is managed using medications (oral, intravenous, or regional anesthesia) to keep the patient comfortable.
- Mobilization: Early mobilization is encouraged to reduce the risk of complications such as blood clots. Physical therapy begins early to restore knee function and mobility.
Expected Outcomes
- Quicker Recovery: Due to the smaller incision, there is typically less blood loss, less trauma to muscles and tissues, and less postoperative pain. This generally leads to a quicker recovery time compared to traditional knee replacement.
- Reduced Scarring: The smaller incision leads to less visible scarring.
- Faster Rehabilitation: Since the quadriceps muscle and tendons are less affected, patients often recover faster and can resume weight-bearing activities sooner.

Key Advantages of MIS TKA:
- Reduced Trauma: Less damage to soft tissues and muscles, which accelerates healing.
- Faster Recovery: Patients typically experience less pain and a quicker return to daily activities.
- Lower Risk of Complications: Reduced risk of infection, blood loss, and blood clots due to smaller incisions and less tissue disruption.
- Improved Cosmesis: Smaller incisions result in less visible scarring.
Considerations:
While MIS TKA offers many advantages, it is not suitable for every patient. Factors like body size, bone quality, and the severity of the joint disease may affect the decision to use MIS techniques. Additionally, the surgeon’s expertise with the minimally invasive approach is crucial for the best outcome.
In conclusion, MIS TKA is a highly effective and less invasive method of knee replacement surgery that offers significant benefits, including reduced recovery time, less pain, and smaller scars, leading to improved patient satisfaction.

